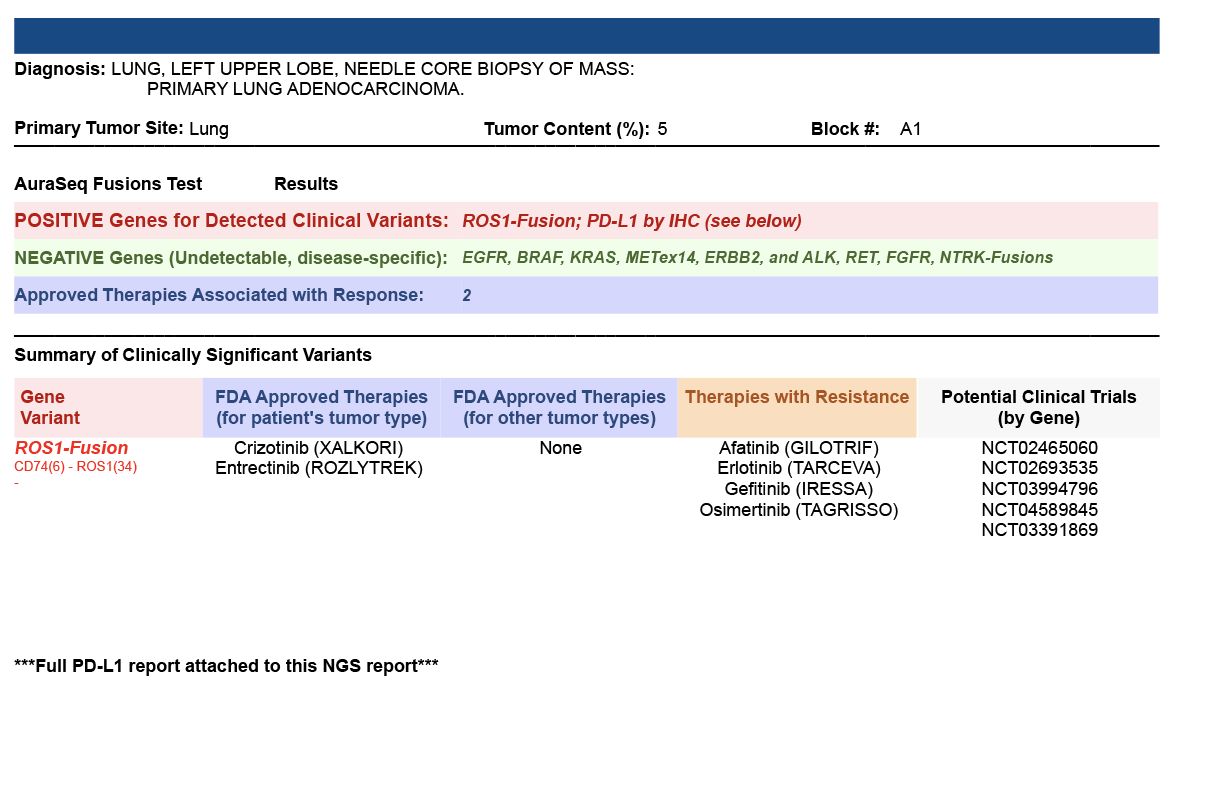
AuraSeq-Fusions panel, a highly multiplexed assay based on an NGS platform, allows the simultaneous identification of drug targets caused by different genomic abnormalities, assisting physicians in selecting personalized therapeutic treatments.
AuraSeq-Fusions panel, a highly multiplexed assay based on an NGS platform, allows the simultaneous identification of drug targets caused by different genomic abnormalities, assisting physicians in selecting personalized therapeutic treatments.
TEST DESCRIPTION
-
The AuraSeq-Fusions panel utilizes Next Generation Sequencing (NGS) and is used to detect cancer-related genomic alterations such as single nucleotide variants (SNVs) and small insertions and deletions (Indels), copy number variants (CNVs) and fusions.
-
This test is intended to detect genomic alterations in several metastatic or advanced cancers, including:
-
Lung adenocarcinoma (NSCLC)
-
Colorectal cancer (CRC)
-
Spitzoid melanoma
-
Glioblastoma multiforme (GBM)
-
Pilocytic astrocytoma
-
Bladder cancer
-
Breast cancer
-
Prostate cancer
-
Soft tissue sarcomas
-
Any other advanced carcinoma that has failed to respond to conventional chemotherapy or is about to start a tyrosine kinase inhibitors (TKIs) regime.
-
Test Methodology
Next Generation Sequencing
Test Performance
-
This assay performs with 100% (95%CI 92.6%-100.0%) sensitivity and 93.8% (95%CI
69.8%-99.8%) specificity. -
The limit of detection (LoD) is 5-6% of mutant DNA in total DNA, at a mean coverage of
1000X and a minimum coverage of 500X. -
Small Indels are detected when present at a minimum frequency of 10% of total DNA, at
a mean coverage of 2000X and a minimum coverage of 500X. -
CNVs can be detected at a minimum gain of 4x on samples with a minimum of 20%
neoplastic nuclei.
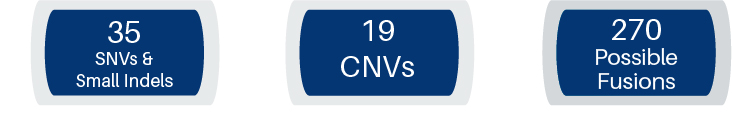
The AuraSeq-Fusions panel is an NGS-based qualitative assay that detects genomic alterations on the 52 genes listed below. The alterations include SNVs and small Indels on 35 genes, CNVs for 19 genes and fusions of 23 different gene moieties with multiple partners covering over 270 possible fusions.
SNVs and Small Indels
| AKT1 | DDR2 | ESR1 | IDH2 | PIK3CA | MAP2K1 |
| ALK | EGFR | FGFR2 | JAK1 | RAF1 | MAP2K2 |
| AR | ERBB2 | FGFR3 | JAK2 | RET | MET |
| BRAF | ERBB3 | GNA11 | JAK3 | ROS1 | MTOR |
| CDK4 | HRAS | GNAQ | KIT | SMO | NRAS |
| CTNNB1 | ERBB4 | IDH1 | PDGFRA | KRAS |
CNVs
| ALK | CDK4 | FGFR1 | KIT | MUCN |
| AR | CDK6 | FGFR2 | KRAS | PDGFRA |
| BRAF | EGFR | FGFR3 | MET | PIK3CA |
| CCND1 | ERBB2 | FGFR4 | MYC | |
|
|
Fusions
| ABL1 | EGFR | ETV5 | NTRK1 | RAF1 |
| ALK | ERBB2 | FGFR1 | NTRK2 | RET |
| AKT3 | ERG | FGFR2 | NTRK3 | ROS1 |
| AXL | ETV1 | FGFR3 | PDGFRA | |
| BRAF | ETV4 | MET | PPARG |
References:
1. Lindeman NI, Cagle PT, Aisner DL, et al. Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors: Guideline From the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. J Mol Diagn. 2018;20(2):129-159.
2. Sepulveda AR, Hamilton SR, Allegra CJ, et al. Molecular Biomarkers for the Evaluation of Colorectal Cancer: Guideline Summary From the American Society for Clinical Pathology, College of American Pathologists, Association for Molecular Pathology, and American Society of Clinical Oncology. J Oncol Pract. 2017;13(5):333-337.
3. Pao, W. Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domain. PLoS Med. 2005;2(3):e73.
4. Dumur CI, Idowu MO, Powers CN. Targeting tyrosine kinases in cancer: the converging roles of cytopathology and molecular pathology in the era of genomic medicine. Cancer Cytopathol. 2013;121(2):61-71.
5. Li MM, Datto M, Duncavage EJ, et al. Standards and Guidelines for the Interpretation and Reporting of Sequence Variants in Cancer: A Joint Consensus Recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J Mol Diagn. 2017;19(1):4-23.
6. Landrum MJ, Lee JM, Benson M, et al. Clin Var: public archive of interpretations of clinically relevant variants. Nucleic Acids Res. 2016; (D1):D862-8.
7. McLaren W, Gil L, Hunt S, et al. The Ensembl Variant Effect Predictor. Genome Biology 2016, 17:122.
TEST ORDERING
Test Reporting (Sample Reporting)
- Variants are reported using a tier system as defined by a joint consensus recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists (5) for the reporting of somatic variants.
-
Tier I: Variants of Strong Clinical Significance (therapeutic, prognostic & diagnostic) with Level A (FDA approved therapies, and included in professional guidelines) or Level B (well-powered studies with consensus from experts in the field, including potential germline pathogenic variants associated with cancer predisposition) evidence.
-
Tier II: Variants of Potential Clinical Significance (therapeutic, prognostic & diagnostic) with Level C (FDA approved therapies for different tumor types or investigational therapies, and/or included in multiple small published studies with some consensus) or Level D (pre-clinic trials or a few case reports without consensus) evidence.
- Tier III: Variants of Unknown Clinical Significance, not observed at significant allele frequency in the general or specific subpopulation databases.
- Tier IV: Benign or likely Benign, observed at significant allele frequency in the general or specific subpopulation databases and no existing published evidence of cancer association. These variants are not reported.